Two types of AMD
Dry AMD
This form is quite common. About 80% (8 out of 10) of people who have AMD have the dry form. Dry AMD is when parts of the macula get thinner with age and tiny clumps of a protein called drusen grow. You slowly lose central vision. There is no way to treat dry AMD yet.
Wet AMD
This form is less common but much more serious. Wet AMD is when new, abnormal blood vessels grow under the retina. These vessels may leak blood or other fluids, causing scarring of the macula. You lose vision faster with wet AMD than with dry AMD.
Many people don’t realize they have AMD until their vision is very blurry. This is why it is important to have regular visits to an ophthalmologist. He or she can look for early signs of AMD before you have any vision problems.
How is AMD Diagnosed and Treated?
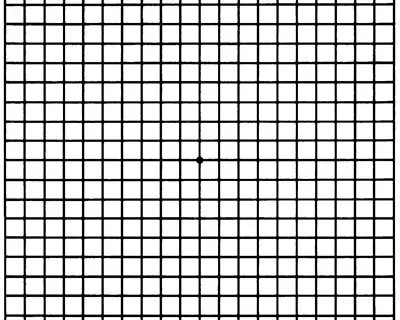
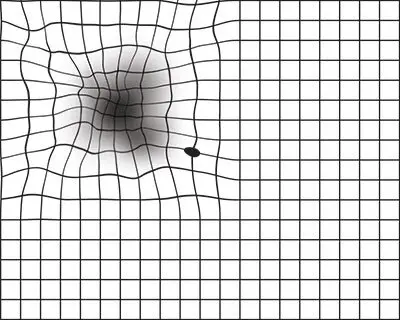
During an eye exam, your ophthalmologist may ask you to look at an Amsler grid. This grid helps you notice any blurry, distorted, or blank spots in your field of vision. Your ophthalmologist will also look inside your eye through a special lens. He or she can see if there are changes in the retina and macula.
Your ophthalmologist will put dilating eye drops in your eye to widen your pupil. This allows him or her to look through a special lens at the inside of your eye.
Your doctor may do fluorescein angiography to see what is happening with your retina. Yellow dye (called fluorescein) is injected into a vein, usually in your arm. The dye travels through your blood vessels. A special camera takes photos of the retina as the dye travels throughout its blood vessels. This shows if abnormal new blood vessels are growing under the retina.
Optical coherence tomography (OCT) is another way to look closely at the retina. A machine scans the retina and provides very detailed images of the retina and macula.
Optical coherence tomography angiography (OCTA) is another way to look closely at the blood vessels in and under the retina. This is like fluorescein angiography but does not use a dye.
Vitamins for AMD
People who have a certain form of age-related macular degeneration (AMD) may benefit from a specific mix of vitamins and minerals. Taking these nutritional supplements might help slow this eye disease.
About 8 out of 10 people with AMD have the dry form. This condition is due to a breakdown or thinning of the macula. Dry AMD usually begins when tiny, yellow deposits called drusen form under the retina. Eventually, the macula may become thinner and stop working properly.
Many people with AMD have drusen. These alone do not cause vision loss. But when drusen grow in size or number, you are at risk for getting early or intermediate AMD. There are not always symptoms with these stages of AMD, though people with intermediate AMD might start to notice a blurred spot in their central vision.
Advanced AMD develops when cells in your macula begin to break down. This is when the blurred spot in your central vision starts getting bigger and darker. That is what robs you of your central vision.
Genetics and Age-Related Macular Degeneration
Age-related macular degeneration (AMD) is the leading cause of irreversible vision loss in the United States. Nearly two million Americans have AMD. This number is projected to more than double over the next two decades.
Anyone can develop AMD, but lifestyle and diet are major factors in an individual's risk. And it's clear that genetic factors have a lot of influence on when AMD might start and how it progresses.
Many Genes Influence AMD Risk, But Two Stand Out
Large genome-wide association studies have identified over 30 genes associated with the risk of developing AMD. These kinds of studies look for genes that are more common in people with certain conditions. If a lot of people have a particular variation of a gene and also have a particular condition—while other people without the variation don’t have the condition—that gene is said to be associated with the condition. Variants in all 30-plus of these genes contribute to different levels of risk of developing AMD.
Variations in two genes have been more closely connected to both developing AMD and whether it progresses to the advanced stages of the disease. These are:
The presence of these genetic variants doesn’t mean that someone will definitely develop AMD. These variants mean that one may have a higher risk of AMD or developing advanced disease in the future.
The complement cascade is an essential part of the body’s immune system. It controls a series of proteins that protect against invading pathogens like bacteria and viruses. Complement can sometimes incorrectly target the body’s healthy cells, including cells in the retina.
Some researchers believe that inflammation and immune mechanisms are part of what causes AMD. The connection between complement gene variants and AMD supports this theory. There are several variants of the complement genes, and they create different levels of AMD risk.
While scientists are intensively researching ARMS2/HTRA1, the role of these genes in AMD is not yet understood. It appears there is a strong connection, but we don’t yet know what these genes do.
Other genes associated with increased AMD risk are involved in cholesterol and lipid (fat) metabolism, collagen production, DNA repair, protein binding, and cell signaling. Research on these genes and their role in disease onset and progression is still underway.
In addition, certain gene variants can have a protective effect against AMD, reducing an individual’s risk of developing the disease. These include variants in other parts of the complement and immune gene groups and other genes that affect lipids.

A retina with soft drusen from dry AMD.
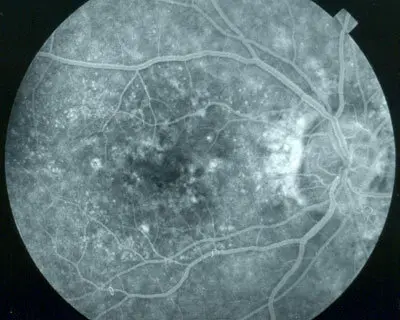
A retina with dry AMD.
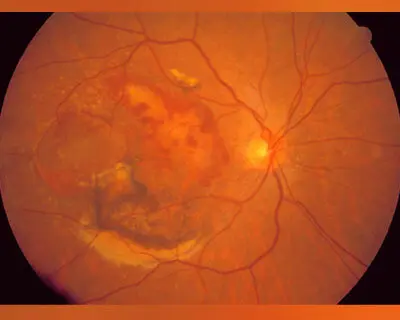
A retina with abnormal, leaking blood vessels of wet AMD.